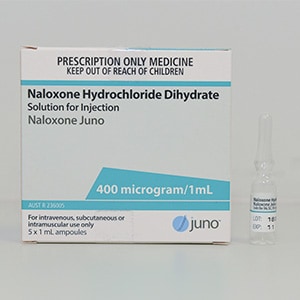
Presentation
400micrograms/mL ampoule
Role
- Management of opioid toxicity with respiratory depression and coma.
- Diagnostic aid in suspected opioid toxicity.
Consultation with a clinical toxicologist is recommended through the local toxicology service or Poisons Information Centre 13 11 26.
Dose
Initial reversal of opioid toxicity
- 50 – 100 micrograms IV q3min PRN
- 800 – 1600micrograms IM q15min PRN
Ongoing reversal of opioid toxicity
4mg naloxone in 100mL sodium chloride 0.9% (40micrograms/mL solution) commenced at the same rate per hour as initial dose required to reverse toxicity.
Reversal of opioid toxicity should aim for:
- Patient rouses to voice
- RR > 9
- Sats > 92% on room air
- pCO2 < 60mmHg
Stocking recommendations
| Tertiary centre | Regional centre | Rural centre | Remote centre |
|---|---|---|---|
| > 25 ampoules | > 25 ampoules | 15 ampoules | 5 ampoules |
Rationale
Naloxone is likely to be readily available in most centres for its reversal of iatrogenic opioid intoxication. Rural centres should carry sufficient stock to reverse initial toxicity.
Precaution
- Due to the short half-life of naloxone (30-90min), opioid toxicity may recur when naloxone wears off. Patients should be observed for at least 2 hours following a single dose of IV naloxone, 4 hours following a single dose of IM naloxone and 6 hours following discontinuation of a naloxone infusion.
- Naloxone may precipitate acute opioid withdrawal in dependant patients.
- Large doses of naloxone may be needed in buprenorphine overdose.
Disclaimer
Fact sheet developed by Queensland Poisons Information Centre.
This fact sheet is about the use of these antidotes in Australia, and may not apply to other countries. Children’s Health Queensland Hospital and Health Service cannot be held responsible for the accuracy of information, omissions of information, or any actions that may be taken as a consequence of reading this fact sheet.